
Low-carbohydrate diets or low-carb diets are dietary programs that restrict carbohydrate consumption, often for the treatment of obesity or diabetes. Foods high in easily digestible carbohydrates (e.g., sugar, bread, pasta) are limited or replaced with foods containing a higher percentage of fats and moderate protein (e.g., meat, poultry, fish, shellfish, eggs, cheese, nuts, and seeds) and other foods low in carbohydrates (e.g., most salad vegetables such as spinach, kale, chard and collards), although other vegetables and fruits (especially berries) are often allowed. The amount of carbohydrate allowed varies with different low-carbohydrate diets.
Such diets are sometimes 'ketogenic' (i.e., they restrict carbohydrate intake sufficiently to cause ketosis). The induction phase of the Atkins diet is ketogenic.
The term "low-carbohydrate diet" is generally applied to diets that restrict carbohydrates to less than 20% of caloric intake, but can also refer to diets that simply restrict or limit carbohydrates to less than recommended proportions (generally less than 45% of total energy coming from carbohydrates).
Low-carbohydrate diets are used to treat or prevent some chronic diseases and conditions, including cardiovascular disease, metabolic syndrome, auto-brewery syndrome, high blood pressure, and diabetes.

Maps, Directions, and Place Reviews
History
Prehistory
A more detailed picture of early human diets before the origin of agriculture may be obtained by analogy to contemporary hunter-gatherers. According to one survey of these societies, a relatively low carbohydrate (22-40% of total energy), animal food-centered diet is preferred "whenever and wherever it [is] ecologically possible", and where plant foods do predominate, carbohydrate consumption remains low because wild plants are much lower in carbohydrate and higher in fiber than modern domesticated crops. Primatologist Katherine Milton, however, has argued that the survey data on which this conclusion is based inflate the animal content of typical hunter-gatherer diets; much of it was based on early ethnography, which may have overlooked the role of women in gathering plant foods. She has also highlighted the diversity of both ancestral and contemporary foraging diets, arguing no evidence indicates humans are especially adapted to a single paleolithic diet over and above the vegetarian diets characteristic of the last 30 million years of primate evolution.
The origin of agriculture brought about a rise in carbohydrate levels in human diets. The industrial age has seen a particularly steep rise in refined carbohydrate levels in Western societies, as well as urban societies in Asian countries, such as India, China, and Japan.
Early dietary science
In 1797, John Rollo reported on the results of treating two diabetic Army officers with a low-carbohydrate diet and medications. A very low-carbohydrate, ketogenic diet was the standard treatment for diabetes throughout the 19th century.
In 1863, William Banting, a formerly obese English undertaker and coffin maker, published "Letter on Corpulence Addressed to the Public", in which he described a diet for weight control giving up bread, butter, milk, sugar, beer, and potatoes. His booklet was widely read, so much so that some people used the term "Banting" for the activity usually called "dieting".
In 1888, James Salisbury introduced the Salisbury steak as part of his high-meat diet, which limited vegetables, fruit, starches, and fats to one-third of the diet.
In the early 1900s Frederick Madison Allen developed a highly restrictive short term regime which was described by Walter R. Steiner at the 1916 annual convention of the Connecticut State Medical Society as The Starvation Treatment of Diabetes Mellitus. People showing very high urine glucose levels were confined to bed and restricted to an unlimited supply of water, coffee, tea, and clear meat broth until their urine was "sugar free"; this took two to four days but sometimes up to eight. After the person's urine was sugar-free food was re-introduced; first only vegetables with less than 5g of carbohydate per day, eventually adding fruits and grains to build up to 3g of carbohydrate per kilogram of body weight. Then eggs and meat were added, building up to 1g of protein/kg of body weight per day, then fat was added to the point where the person stopped losing weight or a maximum of 40 calories of fat per kilogram per day was reached. The process was halted if sugar appeared in the person's urine. This diet was often administered in a hospital in order to better ensure compliance and safety.
Modern low-carbohydrate diets
In 1958, Richard Mackarness M.D. published Eat Fat and Grow Slim, a low-carbohydrate diet with much of the same advice and based on the same theories as those promulgated by Robert Atkins more than a decade later. Mackarness also challenged the "calorie theory" and referenced primitive diets such as the Inuit as examples of healthy diets with a low-carbohydrate and high-fat composition.
In 1967, Irwin Stillman published The Doctor's Quick Weight Loss Diet. The "Stillman diet" is a high-protein, low-carbohydrate, and low-fat diet. It is regarded as one of the first low-carbohydrate diets to become popular in the United States. Other low-carbohydrate diets in the 1960s included the Air Force diet and the drinking man's diet. Austrian physician Wolfgang Lutz published his book Leben Ohne Brot (Life Without Bread) in 1967. However, it was not well known in the English-speaking world.
In 1972, Robert Atkins published Dr. Atkins Diet Revolution, which advocated the low-carbohydrate diet he had successfully used in treating patients in the 1960s (having developed the diet from a 1963 article published in JAMA). The book met with some success, but, because of research at that time suggesting risk factors associated with excess fat and protein, it was widely criticized by the mainstream medical community as being dangerous and misleading, thereby limiting its appeal at the time. Among other things, critics pointed out that Atkins had done little real research into his theories and based them mostly on his clinical work. Later that decade, Walter Voegtlin and Herman Tarnower published books advocating the Paleolithic diet and Scarsdale diet, respectively, each meeting with moderate success.
The concept of the glycemic index was developed in 1981 by David Jenkins to account for variances in speed of digestion of different types of carbohydrates. This concept classifies foods according to the rapidity of their effect on blood sugar levels - with fast-digesting simple carbohydrates causing a sharper increase and slower-digesting complex carbohydrates, such as whole grains, a slower one. The concept has been extended to include the amount of carbohydrate actually absorbed, as well, as a tablespoonful of cooked carrots is less significant overall than a large baked potato (effectively pure starch, which is efficiently absorbed as glucose), despite differences in glycemic indices.
1990s - present
In the 1990s, Atkins published an update from his 1972 book, Dr. Atkins New Diet Revolution, and other doctors began to publish books based on the same principles. This has been said to be the beginning of what the mass media call the "low carb craze" in the United States. During the late 1990s and early 2000s, low-carbohydrate diets became some of the most popular diets in the US. By some accounts, up to 18% of the population was using one type of low-carbohydrate diet or another at the peak of their popularity, and this use spread to many countries. Food manufacturers and restaurant chains like Krispy Kreme noted the trend, as it affected their businesses. Parts of the mainstream medical community has denounced low-carbohydrate diets as being dangerous to health, such as the AHA in 2001, the American Kidney Fund in 2002, Low-carbohydrate advocates did some adjustments of their own, increasingly advocating controlling fat and eliminating trans fat.
Proponents who appeared with new diet guides at that time like the Zone diet intentionally distanced themselves from Atkins and the term 'low carb' because of the controversies, though their recommendations were based on largely the same principles . It can be controversial which diets are low-carbohydrate and which are not. The 1990s and 2000s saw the publication of an increased number of clinical studies regarding the effectiveness and safety (pro and con) of low-carbohydrate diets (see low-carbohydrate diet medical research).
In the United States, the diet has continued to garner attention in the medical and nutritional science communities, and also inspired a number of hybrid diets that include traditional calorie-counting and exercise regimens. Other low-carb diets, such as the Paleo Diet, focus on the removal of certain foods from the diet, such as sugar and grain. On September 2, 2014 a small randomized trial by the NIH of 148 men and women comparing a low-carbohydrate diet with a low fat diet without calorie restrictions over one year showed that participants in the low-carbohydrate diet had greater weight loss than those on the low-fat diet. The low-fat group lost weight, but appeared to lose more muscle than fat.
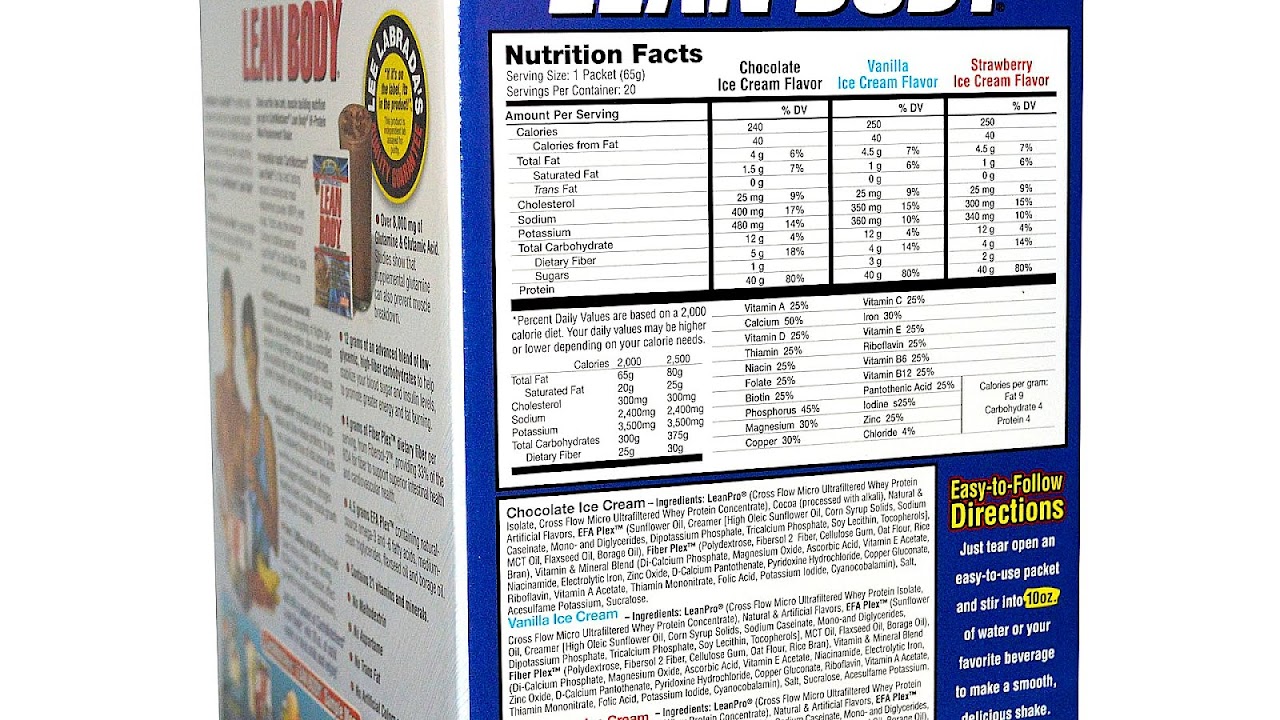
Carb Watchers Lean Body Video
Definition
No consensus definition exists of what precisely constitutes a low-carbohydrate diet. Medical researchers and diet advocates may define different levels of carbohydrate intake when specifying low-carbohydrate diets.
The American Academy of Family Physicians defines low-carbohydrate diets as diets that restrict carbohydrate intake to 20 to 60 grams per day, typically less than 20% of caloric intake.
The body of research underpinning low-carbohydrate diets has grown significantly in the decades of the 1990s and 2000s. Most research centers on the relationship between carbohydrate intake and blood sugar levels (i.e., blood glucose), as well as the two primary hormones produced in the pancreas, that regulate the blood sugar level, insulin, which lowers it, and glucagon, which raises it.

Practices
Low-carbohydrate diets in general recommend reducing nutritive carbohydrates, commonly referred to as "net carbs", i.e., grams of total carbohydrates reduced by the non-nutritive carbohydrates to very low levels. This means sharply reducing consumption of desserts, breads, pastas, potatoes, rice, and other sweet or starchy foods. Some recommend levels less than 20 g of "net carbs" per day, at least in the early stages of dieting (for comparison, a single slice of white bread typically contains 15 g of carbohydrate, almost entirely starch). By contrast, the U.S. Institute of Medicine recommends a minimum intake of 130 g of carbohydrate per day. The FAO and WHO similarly recommend that the majority of dietary energy come from carbohydrates.
Although low-carbohydrate diets are most commonly discussed as a weight-loss approach, some experts have proposed using low-carbohydrate diets to mitigate or prevent diseases, including diabetes, metabolic disease, and epilepsy. Some low-carbohydrate proponents and others argue that the rise in carbohydrate consumption, especially refined carbohydrates, caused the epidemic levels of many diseases in modern society, including metabolic disease and type 2 diabetes.
A category of diets is known as low-glycemic-index diets (low-GI diets) or low-glycemic-load diets (low-GL diets), in particular the Low GI Diet. In reality, low-carbohydrate diets can also be low-GL diets (and vice versa) depending on the carbohydrates in a particular diet. In practice, though, "low-GI"/"low-GL" diets differ from "low-carb" diets in the following ways: First, low-carbohydrate diets treat all nutritive carbohydrates as having the same effect on metabolism, and generally assume their effect is predictable. Low-GI/low-GL diets are based on the measured change in blood glucose levels in various carbohydrates - these vary markedly in laboratory studies. The differences are due to poorly understood digestive differences between foods. However, as foods influence digestion in complex ways (e.g., both protein and fat delay absorption of glucose from carbohydrates eaten at the same time) it is difficult to even approximate the glycemic effect (e.g., over time or even in total in some cases) of a particular meal.
The low-insulin-index diet, is similar, except it is based on measurements of direct insulemic responses i.e., the amount of insulin in the bloodstream to food rather than glycemic response the amount of glucose in the bloodstream. Although such diet recommendations mostly involve lowering nutritive carbohydrates, some low-carbohydrate foods are discouraged, as well (e.g., beef). Insulin secretion is stimulated (though less strongly) by other dietary intake. Like glycemic-index diets, predicting the insulin secretion from any particular meal is difficult, due to assorted digestive interactions and so differing effects on insulin release.

Ketosis and insulin synthesis: what is normal?
A perception developed that getting energy chiefly from dietary protein rather than carbohydrates causes liver damage and that getting energy chiefly from dietary fats rather than carbohydrates causes heart disease and other health problems. This view is still held by the majority of those in the medical and nutritional science communities. However, it is now widely recognized that periodic ketosis is normal, and that ketosis provides a number of benefits, including neuroprotection against diverse types of cellular injury.
People critical of low-carbohydrate diets cite hypoglycemia and ketoacidosis as risk factors. While mild acidosis may be a side effect when beginning a ketogenic diet, no known health emergencies have been recorded. It should not be conflated with diabetic ketoacidosis, which can be life-threatening.
A diet very low in starches and sugars induces several adaptive responses. Low blood glucose causes the pancreas to produce glucagon, which stimulates the liver to convert stored glycogen into glucose and release it into the blood. When liver glycogen stores are exhausted, the body starts using fatty acids instead of glucose. The brain cannot use fatty acids for energy, and instead uses ketones produced from fatty acids by the liver. By using fatty acids and ketones as energy sources, supplemented by conversion of proteins to glucose (gluconeogenesis), the body can maintain normal levels of blood glucose without dietary carbohydrates.
Most advocates of low-carbohydrate diets, such as the Atkins diet, argue that the human body is adapted to function primarily in ketosis. They argue that high insulin levels can cause many health problems, most significantly fat storage and weight gain. They argue that the purported dangers of ketosis are unsubstantiated (some of the arguments against ketosis result from confusion between ketosis and ketoacidosis, which is a mostly diabetic condition unrelated to dieting or low-carbohydrate intake). They also argue that fat in the diet contributes to heart disease only in the presence of high insulin levels and that if the diet is instead adjusted to induce ketosis, fat and cholesterol in the diet are beneficial. Most low-carb diet plans discourage consumption of trans fat.
On a high-carbohydrate diet, glucose is used by cells in the body for the energy needed for their basic functions, and about two-thirds of body cells require insulin to use glucose. Excessive amounts of blood glucose are thought to be a primary cause of the complications of diabetes, when glucose reacts with body proteins (resulting in glycosolated proteins) and change their behavior. Perhaps for this reason, the amount of glucose tightly maintained in the blood is quite low. Unless a meal is very low in starches and sugars, blood glucose will rise for a period of an hour or two after a meal. When this occurs, beta cells in the pancreas release insulin to cause uptake of glucose into cells. In liver and muscle cells, more glucose is taken in than is needed and stored as glycogen (once called 'animal starch'). Diets with a high starch/sugar content, therefore, cause release of more insulin, and so more cell absorption. In diabetics, glucose levels vary in time with meals and vary a little more as a result of high-carbohydrate meals. In nondiabetics, blood-sugar levels are restored to normal levels within an hour or two, regardless of the content of a meal.
However, the ability of the body to store glycogen is finite. Once liver and muscular stores are filled to the maximum, adipose tissue (subcutaneous and visceral fat stores) becomes the site of sugar storage in the form of fat. The body's ability to store fat is almost limitless, hence the modern problem of morbid obesity.
While any diet devoid of essential fatty acids (EFAs) and essential amino acids (EAAs) will result in eventual death, a diet completely without carbohydrates can be maintained indefinitely because triglycerides (which make up fat stored in the body and dietary fat) include a (glycerol) molecule which the body can easily convert to glucose. It should be noted that the EFAs and all amino acids are structural building blocks, not inherent fuel for energy. However, a very-low-carbohydrate diet (less than 20 g per day) may negatively affect certain biomarkers and produce detrimental effects in certain types of individuals (for instance, those with kidney problems). The opposite is also true; for instance, clinical experience suggests very-low-carbohydrate diets for patients with metabolic syndrome.

Studies on health effects
Because of the substantial controversy regarding low-carbohydrate diets and even disagreements in interpreting the results of specific studies, it is difficult to objectively summarize the research in a way that reflects scientific consensus. Although some research has been done throughout the 20th century, most directly relevant scientific studies have occurred in the 1990s and early 2000s. Researchers and other experts have published articles and studies that run the gamut from promoting the safety and efficacy of these diets to questioning their long-term validity to outright condemning them as dangerous. A significant criticism of the diet trend was that no studies evaluated the effects of the diets beyond a few months. However, studies emerged which evaluate these diets over much longer periods, controlled studies as long as two years and survey studies as long as two decades.
A systematic review published in 2014 included 19 trials with a total of 3,209 overweight and obese participants, some with diabetes. The review included both extreme low carbohydrate diets high in both protein and fat, as well as less extreme low carbohydrate diets that are high in protein but with recommended intakes of fat. The authors found that when the amount of energy (kilojoules/calories) consumed by people following the low carbohydrate and balanced diets (45 to 65% of total energy from carbohydrates, 25 to 35% from fat, and 10 to 20% from protein) was similar, there was no difference in weight loss after 3 to 6 months and after 1 to 2 years in those with and without diabetes. For blood pressure, cholesterol levels and diabetes markers there was also no difference detected between the low carbohydrate and the balanced diets. The follow-up of these trials was no longer than two years, which is too short to provide an adequate picture of the long term risk of following a low carbohydrate diet.
Weight loss
A 2003 meta-analysis that included randomized controlled trials found that "low-carbohydrate, non-energy-restricted diets appear to be at least as effective as low-fat, energy-restricted diets in inducing weight loss for up to one year." A 2007 JAMA study comparing the effectiveness of the Atkins low-carb diet to several other popular diets concluded, "In this study, premenopausal overweight and obese women assigned to follow the Atkins diet, which had the lowest carbohydrate intake, lost more weight and experienced more favorable overall metabolic effects at 12 months than women assigned to follow the Zone, Ornish, or LEARN diets." A July 2009 study of existing dietary habits associated a low-carbohydrate diet with obesity, although the study drew no explicit conclusion regarding the cause: whether the diet resulted in the obesity or the obesity motivated people to adopt the diet. A 2013 meta-analysis that included only randomized controlled trials with one year or more of follow-up found, "Individuals assigned to a very low carbohydrate ketogenic diet achieve a greater weight loss than those assigned to a low fat diet in the long term." In 2013, after reviewing 16,000 studies, Sweden's Council on Health Technology Assessment concluded low-carbohydrate diets are more effective as a means to reduce weight than low-fat diets, over a short period of time (six months or less). However, the agency also concluded, over a longer span (12-24 months), no differences occur in effects on weight between strict or moderate low-carb diets, low-fat diets, diets high in protein, Mediterranean diet, or diets aiming at low glycemic indices.
In one theory, one of the reasons people lose weight on low-carbohydrate diets is related to the phenomenon of spontaneous reduction in food intake.
Carbohydrate restriction may help prevent obesity and type 2 diabetes, as well as atherosclerosis.
Blood lipids
Potential favorable changes in triglyceride and high-density lipoprotein cholesterol values should be weighed against potential unfavorable changes in low-density lipoprotein cholesterol and total cholesterol values when low-carbohydrate diets to induce weight loss are considered. However, the type of LDL cholesterol should also be taken into account here, as it could be that small, dense LDL is decreased and larger LDL molecules are increased with low-carb diets. The health effects of the different molecules are still being elucidated, and many cholesterol tests do not account for such details, but small, dense LDL is thought to be problematic and large LDL is not. A 2008 systematic review of randomized controlled studies that compared low-carbohydrate diets to low-fat/low-calorie diets found the measurements of weight, HDL cholesterol, triglyceride levels, and systolic blood pressure were significantly better in groups that followed low-carbohydrate diets. The authors of this review also found a higher rate of attrition in groups with low-fat diets, and concluded, "evidence from this systematic review demonstrates that low-carbohydrate/high-protein diets are more effective at six months and are as effective, if not more, as low-fat diets in reducing weight and cardiovascular disease risk up to one year", but they also called for more long-term studies.
Mortality
A study of more than 100,000 people over more than 20 years within the Nurses' Health Study observationally concluded a low-carbohydrate diet high in vegetables, with a large proportion of proteins and oils coming from plant sources, decreases mortality with a hazard ratio of 0.8. In contrast, a low-carbohydrate diet with largely animal sources of protein and fat increases mortality, with a hazard ratio of 1.1. This study, however, has been met with criticism, due to the unreliability of the self-administered food frequency questionnaire, as compared to food journaling, as well as classifying "low-carbohydrate" diets based on comparisons to the group as a whole (decile method) rather than surveying dieters following established low-carb dietary guidelines like the Atkins or Paleo diets.

Opinions from major governmental and medical organizations
Opinions regarding low-carbohydrate diets vary throughout the medical and nutritional science communities, yet government bodies, and medical and nutritional associations, have generally opposed this nutritional regimen. Since 2003, some organizations have gradually begun to relax their opposition to the point of cautious support for low-carbohydrate diets. Some of these organizations receive funding from the food industry. Official statements from some organizations:
The AAFP released a 'discussion paper' on the Atkins diet in 2006. The paper expresses reservations about the Atkins plan, but acknowledges it as a legitimate weight-loss approach.
The ADA revised its Nutrition Recommendations and Interventions for Diabetes in 2008 to acknowledge low-carbohydrate diets as a legitimate weight-loss plan. The recommendations fall short of endorsing low-carbohydrate diets as a long-term health plan, and do not give any preference to these diets. Nevertheless, this is perhaps the first statement of support, albeit for the short term, by a medical organization. In its 2009 publication of Clinical Practice Recommendations, the ADA again reaffirmed its acceptance of carbohydrate-controlled diets as an effective treatment for short-term (up to one year) weight loss among obese people suffering from type two diabetes.
As of 2003 in commenting on a study in the Journal of the American Medical Association, a spokesperson for the American Dietetic Association reiterated the association's belief that "there is no magic bullet to safe and healthful weight loss." The Association specifically endorses the high-carbohydrate diet recommended by the National Academy of Sciences. They have stated "Calories cause weight gain. Excess calories from carbohydrates are not any more fattening than calories from other sources. Despite the claims of low-carb diets, a high-carbohydrate diet does not promote fat storage by enhancing insulin resistance."
As of 2008 the AHA states categorically that it "doesn't recommend high-protein diets." A science advisory from the association further states the association's belief that these diets "may be associated with increased risk for coronary heart disease." The AHA has been one of the most adamant opponents of low-carbohydrate diets. Dr. Robert Eckel, past president, noted that a low-carbohydrate diet could potentially meet AHA guidelines if it conformed to the AHA guidelines for low fat content.
The position statement by the Heart Foundation regarding low-carbohydrate diets states, "the Heart Foundation does not support the adoption of VLCARB diets for weight loss." Although the statement recommends against use of low-carbohydrate diets, it explains their major concern is saturated fats as opposed to carbohydrate restriction and protein. Moreover, other statements suggest their position might be re-evaluated in the event of more evidence from longer-term studies.
The consumer advice statements of the NHS regarding low-carbohydrate diets state that "eating a high-fat diet could increase your risk of heart disease" and "try to ensure starchy foods make up about a third of your diet"
In 2008, the Socialstyrelsen in Sweden altered its standing regarding low-carbohydrate diets. Although formal endorsement of this regimen has not yet appeared, the government has given its formal approval for using carbohydrate-controlled diets for medically supervised weight loss.
In a recommendation for diets suitable for diabetes patients published in 2011 a moderate low-carb option (30-40%) is suggested.
The HHS issues consumer guidelines for maintaining heart health which state regarding low-carbohydrate diets that "they're not the route to healthy, long-term weight management."
Dietetics Association of Australia
The DAA, gives the following advice in its topic article, "Low Carbohydrate High Fat Diets For Diabetes":
"A Low Carbohydrate, High Fat diet may be used by some nutrition professionals in the short term to achieve particular health goals, but the effectiveness and safety of the diet has not been examined in the longer term. An argument for the use of the diet can potentially be supported by 'established principles in biochemistry and physiology', however long-term randomised controlled trials with consistent dietary methodology are lacking. [...] DAA believes more research is required on the safety and efficacy of such as diet, in people with diabetes and the general population. What we do know from the evidence is that eating a wide variety of nutritious foods, in the right amounts, is crucial to optimal health."

Research
Low-carbohydrate diets became a major weight loss and health maintenance trend during the late 1990s and early 2000s. While their popularity has waned recently from its peak, they remain popular. This diet trend has stirred major controversies in the medical and nutritional sciences communities and, as yet, there is not a general consensus on their efficacy or safety. Many in the medical community remain generally opposed to these diets for long term health although there has been a recent softening of this opposition by some organizations.
Synopsis
Because of the substantial controversy regarding low-carbohydrate diets, and even disagreements in interpreting the results of specific studies, it is difficult to objectively summarize the research in a way that reflects scientific consensus.
Although there has been some research done throughout the twentieth century, most directly relevant scientific studies have occurred in the 1990s and early 2000s and, as such, are relatively new and the results are still debated in the medical community. Supporters and opponents of low-carbohydrate diets frequently cite many articles (sometimes the same articles) as supporting their positions. One of the fundamental criticisms of those who advocate the low-carbohydrate diets has been the lack of long-term studies evaluating their health risks. This has begun to change as longer term studies are emerging.
Meta-analytic summaries
A 2012 systematic review studying the effects of low-carbohydrate diet on weight loss and cardiovascular risk factors showed the LCD to be associated with significant decreases in body weight, body mass index, abdominal circumference, blood pressure, triglycerides, fasting blood sugar, blood insulin and plasma C-reactive protein, as well as an increase in high-density lipoprotein cholesterol (HDL). Low-density lipoprotein cholesterol (LDL) and creatinine did not change significantly. The study found the LCD was shown to have favorable effects on body weight and major cardiovascular risk factors (but concluded the effects on long-term health are unknown). The study did not compare health benefits of LCD to low-fat diets.
A meta-analysis published in the American Journal of Clinical Nutrition in 2013 compared low-carbohydrate, Mediterranean, vegan, vegetarian, low-glycemic index, high-fiber, and high-protein diets with control diets. The researchers concluded that low-carbohydrate, Mediterranean, low-glycemic index, and high-protein diets are effective in improving markers of risk for cardiovascular disease and diabetes.

Criticism and controversies
Water-related weight loss
In the first week or two of a low-carbohydrate diet, much of the weight loss comes from eliminating water retained in the body. The presence of insulin in the blood fosters the formation of glycogen stores in the body, and glycogen is bound with water, which is released when insulin and blood sugar drop. A ketogenic diet is known to cause dehydration as an early, temporary side-effect.
Exercise
Advocates of low-carbohydrate diets generally dispute any suggestion that such diets cause weakness or exhaustion (except in the first few weeks as the body adjusts), and indeed most highly recommend exercise as part of a healthy lifestyle. A large body of evidence stretching back to the 1880s shows that physical performance is not negatively affected by ketogenic diets once a person has been accustomed to such a diet.
Arctic cultures, such as the Inuit, were found to lead physically demanding lives consuming a diet of about 15-20% of their calories from carbohydrates, largely in the form of glycogen from the raw meat they consumed. However, studies also indicate that while low-carb diets will not reduce endurance performance after adapting, they will probably deteriorate anaerobic performance such as strength-training or sprint-running because these processes rely on glycogen for fuel.
Vegetables and fruits
Many critics argue that low-carbohydrate diets inherently require minimizing vegetable and fruit consumption, which in turn robs the body of important nutrients. Some critics imply or explicitly argue that vegetables and fruits are inherently all heavily concentrated sources of carbohydrates (so much so that some sources treat the words 'vegetable' and 'carbohydrate' as synonymous). While some fruits may contain relatively high concentrations of sugar, most are largely water and not particularly calorie-dense. Thus, in absolute terms, even sweet fruits and berries do not represent a significant source of carbohydrates in their natural form, and also typically contain a good deal of fiber which attenuates the absorption of sugar in the gut. Lastly, most of the sugar in fruit is fructose, which has a reported negligible effect on insulin levels in obese subjects.
Most vegetables are low- or moderate-carbohydrate foods (in the context of these diets, fiber is excluded because it is not a nutritive carbohydrate). Some vegetables, such as potatoes and carrots, have high concentrations of starch, as do corn and rice. Most low-carbohydrate diet plans accommodate vegetables such as broccoli, spinach, cauliflower, and peppers. The Atkins diet recommends that most dietary carbs come from vegetables. Nevertheless, debate remains as to whether restricting even just high-carbohydrate fruits, vegetables, and grains is truly healthy.
Contrary to the recommendations of most low-carbohydrate diet guides, some individuals may choose to avoid vegetables altogether to minimize carbohydrate intake. Low-carbohydrate vegetarianism is also practiced.
Raw fruits and vegetables are packed with an array of other protective chemicals, such as vitamins, flavonoids, and sugar alcohols. Some of those molecules help safeguard against the over-absorption of sugars in the human digestive system. Industrial food raffination depletes some of those beneficial molecules to various degrees, including almost total removal in many cases.
Micronutrients and vitamins
The major low-carbohydrate diet guides generally recommend multivitamin and mineral supplements as part of the diet regimen, which may lead some to believe these diets are nutritionally deficient. The primary reason for this recommendation is that if the switch from a high-carbohydrate to a low-carbohydrate, ketogenic diet is rapid, the body can temporarily go through a period of adjustment during which it may require extra vitamins and minerals. This is because the body releases excess fluids stored during high-carbohydrate eating. In other words, the body goes through a temporary "shock" if the diet is changed to low-carbohydrate quickly, just as it would changing to a high-carbohydrate diet quickly. This does not, in and of itself, indicate that either type of diet is nutritionally deficient. While many foods rich in carbohydrates are also rich in vitamins and minerals, many low-carbohydrate foods are similarly rich in vitamins and minerals.
Glucose availability
A common argument in favor of high-carbohydrate diets is that most carbohydrates break down readily into glucose in the bloodstream, and therefore the body does not have to work as hard to get its energy in a high-carbohydrate diet as a low-carbohydrate diet. This argument, by itself, is incomplete. Although many dietary carbohydrates do break down into glucose, most of that glucose does not remain in the bloodstream for long. Its presence stimulates the beta cells in the pancreas to release insulin, which has the effect of causing about two-thirds of body cells to take in glucose, and causing fat cells to take in fatty acids and store them. As the blood-glucose level falls, the amount of insulin released is reduced; the entire process is completed in non-diabetics in an hour or two after eating. High-carbohydrate diets require more insulin production and release than low-carbohydrate diets, and some evidence indicates the increasingly large percentage of calories consumed as refined carbohydrates is positively correlated with the increased incidence of metabolic disorders such as type 2 diabetes.
In addition, this claim neglects the nature of the carbohydrates ingested. Some are indigestible in humans (e.g., cellulose), some are poorly digested in humans (e.g., the amylose starch variant), and some require considerable processing to be converted to absorbable forms. In general, uncooked or unprocessed (e.g., milling, crushing, etc.) foods are harder (typically much harder) to absorb, so do not raise glucose levels as much as might be expected from the proportion of carbohydrate present. Cooking (especially moist cooking above the temperature necessary to expand starch granules) and mechanical processing both considerably raise the amount of absorbable carbohydrate and reduce the digestive effort required.
Analyses which neglect these factors are misleading and will not result in a working diet, or at least one which works as intended. In fact, some evidence indicates the human brain - the largest consumer of glucose in the body - can operate more efficiently on ketones (as efficiency of source of energy per unit oxygen).
Resistant starch
The restriction of starchy plants, by definition, severely limits the dietary intake of microbiota accessible carbohydrates and may negatively affect the microbiome in ways that contribute to disease. Starchy plants, in particular, are a main source of resistant starch -- an important dietary fiber with strong prebiotic properties. Resistant starches are not digestible by mammals and are fermented and metabolized by gut flora into short chain fatty acids, which are well known to offer a wide range of health benefits. Resistant starch consumption has been shown to improve intestinal/colonic health, blood sugar, glucose tolerance, insulin-sensitivity and satiety. Public health authorities and food organizations such as the Food and Agricultural Organization, the World Health Organization, the British Nutrition Foundation and the U.S. National Academy of Sciences recognize resistant starch as a beneficial carbohydrate. The Joint Food and Agricultural Organization of the United Nations/World Health Organization Expert Consultation on Human Nutrition stated, "One of the major developments in our understanding of the importance of carbohydrates for health in the past twenty years has been the discovery of resistant starch."
Other controversies
In 2004, the Canadian government ruled that foods sold in Canada could not be marketed with reduced or eliminated carbohydrate content as a selling point, because reduced carbohydrate content was not determined to be a health benefit. The government ruled that existing "low carb" and "no carb" packaging would have to be phased out by 2006.
Some variants of low-carbohydrate diets involve substantially lowered intake of dietary fiber, which can result in constipation if not supplemented. For example, this has been a criticism of the induction phase of the Atkins diet (the Atkins diet is now clearer about recommending a fiber supplement during induction).
Source of the article : Wikipedia

EmoticonEmoticon